Abstract
Introduction: Novel targeted therapies greatly improved outcomes of patients with chronic lymphocytic leukemia (CLL). Among these, ibrutinib is the only one approved in the front-line (1L) setting for patients with or without del(17p) or TP53 mutations. This study aims to compare healthcare resource utilization (HRU), costs, and time to next treatment (TTNT), following initiation of 1L ibrutinib single agent versus CIT and in particular bendamustine/rituximab (BR), in real-world.
Methods: The Optum Clinformatics® Extended DataMart De-Identified Databases (01/2004-06/2017) was used to identify adults with CLL diagnosis initiating 1L ibrutinib single agent or CIT (index date) on 02/12/2014 or after. For CIT, only combinations of chemotherapy and CD20 antibody agents recommended by the National Comprehensive Cancer Network guidelines were considered. Patients were also required to have ≥12 months and ≥30 days of continuous eligibility pre- and post-index date, respectively. For each comparison, patients' baseline characteristics were balanced using inverse probability of treatment weighting (IPTW). HRU, costs, and TTNT, were evaluated over 1L therapy. Mean monthly cost differences (MMCD) and rate ratios (RR) obtained from generalized linear models were used to compare costs and HRU, respectively, along with 500-sample bootstrap confidence intervals and P-values. TTNT was defined as the time from initiation of 1L treatment to the initiation of a new antineoplastic agent that was not part of the 1L regimen. TTNT comparisons were performed using Kaplan-Meier (KM) curves with log-rank tests. The hazards of initiating a new treatment were compared between the cohorts using hazard ratios (HRs) obtained from Cox models.
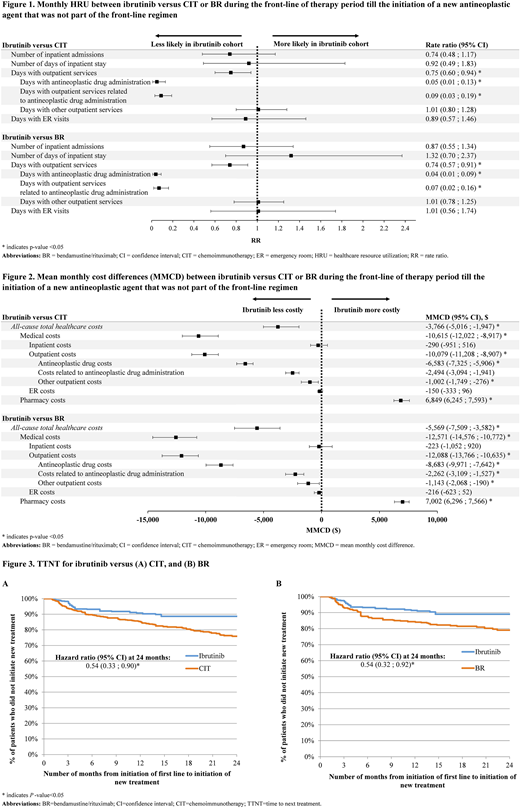
Results: Of 1,161 1L patients, 322 initiated ibrutinib and 839 initiated CIT, including 455 on BR. After IPTW, cohorts had comparable baseline characteristics. CIT patients had significantly more days with outpatient (OP) services (RR=0.75; P<0.05), mainly driven by antineoplastic drug administration-related OP visits (Fig.1; P<0.0001). Ibrutinib patients incurred significantly higher pharmacy costs (MMCD=$6,849; P<0.0001) that were fully offset by lower medical costs (MMCD=-$10,615; P<0.0001), resulting in net monthly total cost reduction of $3,766 (P<0.0001; Fig. 2) vs. CIT patients. While no significant difference was observed in the number of days with other OP visits (i.e., not related to antineoplastic treatment), the corresponding cost was significantly lower in ibrutinib patients (MMCD=-$1,002; P=0.0120).
Ibrutinib patients also had fewer OP visits compared to BR patients, mainly due to drug administration-related OP visits (Fig. 1). Relative to BR, ibrutinib patients' higher pharmacy costs (MMCD=$7,002; P<0.0001) were fully offset by lower medical costs (MMCD=-$12,571; P<0.0001), yielding monthly reduction in the total cost of care of $5,569 (P<0.0001; Fig. 2).
KM analysis of TTNT revealed that, at 24 months post-index, 88.6% of ibrutinib patients did not initiate a new treatment compared to 75.9% among CIT patients (log-rank P=0.0347; Fig. 3A). The hazard of initiating a new treatment was also lower for ibrutinib when compared to CIT, with significant HRs of 0.30 (P=0.0045), 0.59 (P=0.0415), and 0.54 (P=0.0171) at 3, 18, and 24 months post-index, respectively (Fig. 3A). The proportion of patients who did not initiate a new treatment 24 months post-index was significantly higher in ibrutinib cohort than in BR cohort (89.0% versus 79.0%; log-rank P=0.0421). The hazard of initiating a new treatment was also lower for ibrutinib compared to BR, with significant HRs of 0.40 (P=0.0449), 0.54 (P=0.0410), 0.55 (P=0.0360), 0.57 (P=0.0346), and 0.54 (P=0.0219) at 3, 9, 12, 18, and 24 months post-index, respectively (Fig. 3B).
Conclusion: During 1L CLL treatment, ibrutinib patients had higher pharmacy costs that were fully offset by lower medical costs, resulting in net total cost reduction compared to CIT or BR patients. In addition to fewer OP visits and lower OP costs related to the antineoplastic treatment, ibrutinib was also associated with lower cost in other OP services. TTNT was significantly longer among ibrutinib patients vs. CIT or BR patients. Furthermore, consistent with the high rates of progression-free survival observed among ibrutinib patients in clinical trials, nearly 90% of patients did not initiate a new treatment after 24 months of follow-up.
Wang:Janssen Scientific Affairs, LLC: Employment, Equity Ownership. Emond:Janssen Scientific Affairs, LLC: Research Funding. Romdhani:Janssen Scientific Affairs, LLC: Research Funding. Lefebvre:Janssen Scientific Affairs, LLC: Research Funding. Sundaram:Johnson & Johnson: Employment, Equity Ownership, Other: Travel; AbbVie: Employment, Equity Ownership, Other: Travel. Mato:TG Therapeutics: Research Funding; Regeneron: Research Funding; Pharmacyclics: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Sunesis: Honoraria, Research Funding; Prime Oncology: Speakers Bureau; Abbvie: Consultancy; Acerta: Research Funding; AstraZeneca: Consultancy; Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal